Ear Infections and Paediatric Chiropractic Care:
Chiropractors like myself who have a special interest in Paediatric cases commonly see patients daily who present with a variety of non-specific symptoms such as irritability, poor sleep, and poor feeding. A detailed history and close physical examination of these cases can help to evaluate whether these symptoms are indeed due to Acute Otitis Media (AOM), or if they are being caused by another condition/issue.
If you would like to skip the more complex Science parts of this article below, at the end you will find a list of frequently asked questions that I receive from patients regarding Acute Otitis Media.
This article aims to raise awareness of AOM and highlights the relevant anatomy, epidemiology and causes. We discuss the prevention, diagnosis and management of AOM in primary care, the recognition of complications and when to refer to secondary care.
AOM is one of the most common childhood diseases, and is a main cause of medical consultations and antimicrobial prescriptions in developed countries (Venekamp et al. 2014). Even though it is a concern in first world countries like Australia, there is an even greater burden in developing countries due to complications that have a much more significant impact on health. It is estimated by the World Health Organisation (WHO) that approximately 51,000 deaths occur annually in children younger than five years, attributable to complications of AOM (Safadi & Jarovsky 2017).
Even though Otitis Media (OM) is a global problem, the specific number of cases per year is difficult to determine due to the lack of reporting and different incidence across many geographical regions. What we do know is that the peak incidence of OM occurs between the ages of six and twelve months of life and declines after age five. Approximately 80% of all children will experience a case of OM during their lifetime, and between 80% and 90% of all children will have OM with an effusion before school age (Curran et al. 2018; Usonis et al. 2016).
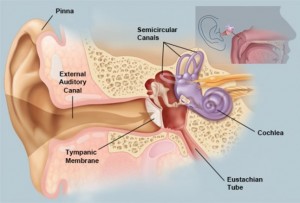
OM initially starts as an inflammatory process following a viral upper respiratory tract infection involving the mucosa of the nose, nasopharynx, and Eustachian Tube. Due to the narrowness of the middle ear, the swelling caused by the inflammatory process obstructs the narrowest part of the Eustachian Tube leading to a decrease in ventilation. This leads to a cascade of events like an increase in negative pressure in the middle ear and a build-up of mucosal secretions. This allows for the colonisation of bacterial and viral organisms in the middle ear. The growth of these microbes in the middle ear then leads to pus formation, which can be seen clinically as bulging of the tympanic membrane (TM) and middle ear fluid (Danishyar & Ashurst 2020).
So how as a parent do you know your child may have AOM? Although one of the best indicators for OM is ear pain, many children can present with non-specific signs and symptoms, which can make the diagnosis challenging. These symptoms include irritability, headache, disturbed or restless sleep, poor feeding, vomiting, failure to thrive, or diarrhoea. Approximately two-thirds of children present with fever, which is typically low grade.
According to guidelines, evidence of moderate to severe bulging of the TM, or new onset of ear discharge, or mild TM bulging with recent onset of ear pain is required for the diagnosis of AOM.
The table from the National Institute for Health and Care Excellence (Curran et al. 2018) lists the more common risk factors associated with AOM.
| Risk factors for AOM | Risk factors for recurrent AOM |
| Young age | Early age of first episode of AOM, especially less than 6 months of age |
| Male sex | Gastro-oesophageal reflux disease |
| Smoking and/or passive smoking (especially mother in children) | Use of dummy |
| Day-care or nursery attendance | Flat, supine feeding |
| Formula feeding (breastfeeding greater or equal to 3 months is protective) | Winter season |
| Craniofacial abnormalities (e.g. Down’s syndrome, cleft palate) |
Frequently asked questions.
What types of treatment are available for my child?
Antibiotics
According to Levi et al. (2013), almost half of all Paediatric antibiotic prescriptions are written for otitis media. Curran et al. (2018) further explains that long-term antibiotics have been shown to reduce the incidence of recurrent AOM, however both the national and international guidelines do not support the use of long-term antibiotics due to potential harm. Patients with a high risk of complications (e.g. immunocompromised) or with suppuration or perforation, or under the age of two should be prescribed antibiotics. Venekamp et al. (2014) further supports that approximately 60% of children’s symptoms improve within 24 hours without the use of antibiotic treatment.
However, the treatment with antibiotics is controversial. Without proper treatment, suppurative fluid from the middle ear can extend to the adjacent anatomical locations and result in complications for example, TM perforation, mastoiditis, hearing loss, meningitis, and others (Danishyar & Ashurst 2020).
- ‘Watch and Wait’ method and symptomatic relief
One of the main recommendations for the treatment of ear infections is “watchful waiting”. However, parents need to administer symptomatic relief. This can be achieved with warm compresses, steam, gargling salt water, decongestant nasal sprays, or simple analgesia (e.g. paracetamol or ibuprofen) to reduce pain and fever (Curran et al. 2018; Levi et al. 2013).
- Probiotics
Probiotics are microorganisms that are thought to confer health benefits by restoring microbial balance. One study yielded results that when probiotics were taken, there was a reduction in the number of episodes in the first 7 months of life. However, there is conflicting evidence on the effectiveness of probiotics in preventing AOM (Levi et al. 2013).
What is the difference between viral AOM and bacterial AOM?
Infection of the middle ear can be due to viral, bacterial or coinfection with both. Infections, allergies and environmental factors may also contribute to OM. The most common bacterial organisms that are responsible for causing more than 95% of cases of OM are: (1) Streptococcus pneumonaie; (2) Haemophilus influenzae (NTHi); (3) Moraxella catarrhalis These organisms are believed to enter the middle ear cleft via the Eustachian Tube (Danishyar & Ashurst 2020; Qureishi et al. 2014).
The most common viral pathogens of OM include: respiratory syncytial virus (RSV), influenza viruses, adenoviruses, human metapneumovirus, and picornaviruses (Danishyar & Ashurst 2020). It is hypothesised that viral infections of the nasopharynx create an environment that promotes bacterial colonisation, adhesion to cells, and invasion of the middle ear (Qureishi et al. 2014).
Why do antibiotics not always work?
Antibiotics are used to treat infections caused by bacteria. However, as explained above, not all ear infections are caused by bacteria. Viruses are different to bacteria; they do not have cell walls and are surrounded by a protective protein coat which makes it impossible for them to be targeted by antibiotics.
Do Grommets work?
Guidelines recommend, in otherwise healthy children with persistent otitis media and effusion, instead of undergoing tube insertion, they should be re-examined at three, six, and twelve-month intervals until effusion is no longer present. This is unless there is significant hearing loss or structural abnormalities of the ear drum and middle ear, tubes should then be considered.
| For Tubes | Against Tubes |
| – Sustained hearing loss >31dB
– Delayed speech/hearing development – Frequent or severe AOM – Allergy to multiple antimicrobials – Exposure to large number of other children |
– Normal or near-normal hearing
– Age-appropriate speech and language – Little or no AOM history – Unilateral effusion – Parental reluctance |
How would I diagnose AOM in clinical practice as a Paediatric Chiropractor?
OM is diagnosed clinically depending on the presenting signs and symptoms combined with objective findings on physical examination. The most common tool used is the pneumatic otoscope, which allows us to observe the motility of the TM and any presence of fluid within the middle ear. In addition, we test children’s hearing and observe for any external swelling, discharge or tenderness. Due to the fact that AOM can present with other symptoms of irritability we can diagnose whether your child’s irritability is due to AOM or another cause.
How can chiropractic care help my child?
In respect to AOM, chiropractic techniques focus on the function of cranial structures in relation to the neck. These structures may directly affect the Eustachian Tube. Another hypothesis is that cervical chiropractic manual therapy (CMT) may have an impact on the lymphatic and muscular systems. This is because lymphatic flow requires muscular contractions, arterial pulsations and external compression of body tissue. Therefore, the upper neck CMT work may reduce tension within tight muscles which increases lymphatic and inner ear canal drainage.
I hope you have enjoyed my article on AOM, If you would like to be kept up to date with all our latest blog posts please “like” our Facebook page.
Allison Kaczmarczyk
B.Sc.(Chiro) M.Clin.Chiro. DACCP (Candidate)
Chiropractor
References
Curran, J.F., Cornwall, H.L., Perenyei, M., & Moorhouse, T. (2018). Acute otitis media. InnovAit, 11(6), 305-312. https://doi.org.10.1177/1755738018766193
Danishyar, A., & Ashurst, J.V. 2020). Acute otitis media. StatPearls [Internet]. Accessed from https://www.ncbi.nlm.nih.gov/books/NBK470332/
Levi, J.R., Brody, R.M., McKee-Cole, K., Pribtikin, E., & O’Reily, R. (2013). Complementary and alternative medicine for pediatric otitis media. International Journal of Pediatric Otorhinolaryngology, 77, 926-931. https://doi.org/10.1016/j.ijporl.2013.03.009
Paradise, J.L., Feldman, H.M., Campbell, T.F., Dollaghan, C.A., Colborn, K., Bernard, B.S., Rockette, H.E., Janosky, J.E., Pitcairn, D.L., Sabo, D.L., Kurs-Lasky, M., & Smith, C.G. (2001). Effect of early or delayed insertion of tympanostomy tubes for persistent otitis media on developmental outcomes at the age of three years. The New England Journal of Medicine, 344(16), 1179-1187. https://doi.org/10.1056/NEJM200104193441601.
Paradise, J.L., Feldman, H.M., Campbell, T.F., Dollaghan, C.A., Rockette, H.E., Pitcairn, D.L., Smith, C.G., Colborn, K., Bernard, B.S., Kurs-Lasky, M., Janosky, J.E., Sabo, D.L., O’Connor, R.E., &Pelham, W.E. (2007). Tympanostomy tubes and developmental outcomes at 9 to 11 years of age. The New England Journal of Medicine, 356(3), 248-261. https://doi.org/10.1056/NEJMoa062980.
Qureishi, A., Lee, Y., Belfield, K., Birchall, J., & Daniel, M. (2014). Update on otitis media – prevention and treatment. Infection and Drug Resistance, 7, 15-24. https://doi.org/10.2147/IDR.S39637
Safadi, M.A.P., & Jarovsky, D. (2017). Acute otitis media in children: a vaccine-preventable disease? Brazilian Journal of Otorhinolaryngology, 83(3), 241-242. https://doi.org/10.1016/j.bjorl.2017.02.004
Venekamp, R.P., Damoiseaux, R.A.M.J., & Schlider, A.G.M. (2014). Acute otitis media in children. BMJ Clinical Evidence, 2014, 1-21. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4166866/
Venekamp, R.P., Mick, P., Schilder, A.G.M., & Nunez, D.A. (2018). Grommets (ventilation tubes) for recurrent acute otitis media in children (review). Cochrane Database of Systematic Reviews, 5, 1-4. https://doi.org/10.1002/14651858.CD012017.pub2